Effect of Positioning of Wheelchair Mounted Headrests During Transportation in a Motor Vehicle on Pediatric Neck Injury Criteria Outcomes
Susan I. Fuhrman, PhD* Patricia E. Karg, MSBME* Gina E. Bertocci, PhD**
* University of Pittsburgh, Department of Rehabilitation Science and Technology
** University of Louisville, Department of Mechanical Engineering
ABSTRACT
The effect of wheelchair-mounted headrest position on neck injury criteria (Nij) outcomes for wheelchairs used as seats in motor vehicles during rear impact was explored in this study using a validated MADYMO computer simulation model. Results support current recommendations to place the headrest as close as possible to the posterior aspect of the head; and that the top of the headrest pad should be placed at least one inch above the superior aspect of the ears. In this study, headrest positioning in compliance with these best practice recommendations reduced the likelihood of pediatric neck injury by reducing the neck injury criteria by up to 100% compared to other positions.
KEYWORDS
neck injury criteria; headrest; wheelchair; rear impact; transportation; pediatric
INTRODUCTION
While the majority of traffic fatalities occur in frontal impact, the majority of injuries in motor vehicle accidents occur in rear impact [1]. Federal motor vehicle safety standards (FMVSS) specify vehicle requirements designed to afford maximum occupant protection. However, wheelchairs are medical devices [2] and are not regulated by the FMVSS, even when the wheelchair is used as a seat in a motor vehicle. The wheelchair-seated vehicle occupant is not protected by federal safety standards that relate specifically to the vehicle seating systems.
The stated purpose and scope of FMVSS 202 - Head Restraints for Passenger Vehicles [3] is to specify “requirements for head restraints to reduce the frequency and severity of neck injury in rear-end and other collisions.” It describes minimum vehicular headrest positioning as well as head restraint strength requirements using either quasi-static testing or dynamic testing. The automotive industry has also developed newer dynamic head restraint systems to increase occupant protection in rear impacts [4].
Incidence of pediatric neck injury from rear impact is not found in the literature for child restraint systems or for children seated on manufacturer installed vehicle seats. We postulate that children’s necks are well protected by either FMVSS 213 [5] compliant child restraints or by the vehicle seatback, which effectively limit rearward head excursion of children due to their shorter stature than adults. Children who remain seated in their wheelchairs while traveling in motor vehicles do not enjoy these same protections, as the wheelchair seatback height is insufficient to limit rearward head excursion.
Wheelchair mounted headrests are primarily designed to provide individuals with improved support, function and comfort. They are not designed with the intent to provide occupant protection within a motor vehicle impact environment, nor are they tested to withstand rear impact conditions. In our research, we found that 80% of pediatric wheelchairs are prescribed with wheelchair-mounted headrests [6]. The Rehabilitation Engineering Research Center on Wheelchair Transportation Safety has published a best practices guideline for headrest placement for travel in a motor vehicle [7] based on automotive occupant protection that recommends that the headrest be placed as close to the posterior aspect of the head as possible with the middle of the headrest aligning with the top of the ears. A comparison of rear impact sled tests conducted with a pediatric wheelchair with and without a headrest indicated that wheelchair mounted headrests have the potential to reduce head and neck injury in rear impact [8].
This study used crash testing and computer simulation modeling to evaluate the effect of wheelchair headrest position on neck injury criteria (Nij) outcomes for pediatric wheelchair-seated motor-vehicle occupants.
METHODS

Figure 1: Baseline MADYMO model of manual pediatric wheelchair, Hybrid III 6-year old ATD, and wheelchair tiedown and occupant restraint system. (Click for larger view)
A MADYMO computer simulation model was developed to represent the dynamic response of a manual pediatric wheelchair with a simple single-pad headrest and a seated Hybrid III 6-year old anthropomorphic test device (ATD) in a moderately severe rear impact (Figure 1). The simulation model was developed based on results from physical sled testing conducted at the University of Michigan Transportation Research Institute using the Quickie Zippie® manual pediatric wheelchair with a slightly modified (no fore-aft adjustment) Sunrise Medical® single-pad headrest. The sled test acceleration time-history data was used in the model to reproduce the 26 km/h, 11g (16 mph, 11 g) rear impact crash pulse. The wheelchair model was built to reproduce the tested wheelchair and headrest. The MADYMO software includes a validated Hybrid III 6-year old ATD model, which was incorporated into the simulation. The simulation model replicated the test setup and incorporated a 4-point strap-type wheelchair tiedown (linear belt elements) and 3-point vehicle-anchored occupant restraint (finite element belts).
The dynamic simulation model results were validated against the sled test responses for tiedown loads, wheelchair center of gravity acceleration, lapbelt loads, ATD chest acceleration, ATD head center of gravity acceleration, and ATD upper neck forces (axial, shear) and bending moments. Using methods developed by Pipkorn and Eriksson [9], the model was validated using four statistical and comparative tests, which included a comparison of mean values, correlation, standard deviation of the residual, and a comparison of the time and peak signal responses. Model validation results indicated that the model matched the sled test result thresholds for 87% of all statistical validation tests, and would be useful for predicting front securement point loads, wheel loads, lapbelt loads, chest acceleration and neck injury criteria (Nij) outcome measures [10].
The validated dynamic simulation model was used to examine the role of headrest position on neck injury. Headrest position was varied independently within the validated model both for headrest proximity to the posterior aspect of the head and for the headrest height relative to the head. The headrest position in the baseline model was located 5 cm behind the head, which is the maximum recommended distance from the head [7]. Headrest proximity was then incremented by 2.5 cm intervals. The closest headrest position was located with the headrest in contact with the posterior aspect of the head (5 cm closer to the back of the head than baseline). To capture headrest positions that may exceed the recommended maximum, a maximum distance of 10 cm was modeled (5 cm beyond the baseline model headrest position). In the vertical direction, the baseline headrest position was configured such that the headrest was initially placed with the midline of the headrest pad vertically aligned with the center of gravity of the head. The headrest vertical position was varied by raising the headrest by 2.5 cm and 5 cm above the baseline, then by lowering it 2.5 and 5 cm below baseline. Dynamic simulations using the MADYMO processor for each headrest configuration yielded neck injury criteria (Nij) outcomes, where Nij is a normalized measure of combined upper neck axial and neck bending moments [11].
This study focused on evaluating and substantiating current clinical best practice guidelines for positioning wheelchair headrests for travel in a vehicle by evaluating the effects of headrest position, both proximity to the posterior aspect of the head and height relative to the head, on neck injury criteria (Nij) outcome measures.
RESULTS

Figure 2: Nij response is displayed for five headrest proximities. Headrest proximity is measured from the anterior surface of the headrest pad. Baseline headrest position is located 5 cm behind the posterior aspect of the head. Baseline Nij value (0.5) is shown in yellow. Head center of gravity is highlighted with a yellow circle. (Click for larger view)
Nij was shown to be strongly dependent on headrest position. Figure 2 displays the Nij outcomes with headrest proximity. The vertical lines indicate the anterior surface of the headrest. A 32% reduction in Nij was achieved by placing the headrest very close to the posterior head surface. Headrest positions 7.5 cm (+2.5 cm with respect to baseline) and 10 cm (+5.0 cm with respect to baseline) behind the head increased Nij by 18% and 31% above the baseline Nij value (Nij = 0.5). Nij references do not indicate a Nij protection reference value for use in determining the likelihood of whiplash-type neck injuries [12]. However, it is anticipated that smaller Nij values would be associated with less likelihood of neck injury. Headrest position located 10 cm behind the head resulted in Nij values two times greater than the Nij value when the headrest is placed in the optimal position directly behind the head.
Figure 3 displays Nij in response to changes in headrest height. The yellow circle indicates the ATD head center of gravity. The ATD head was positioned in the sled tests and modeled such that the head center of gravity was in line with the center of the headrest pad. The headrest pad measures 15 cm (6 inches) in height. The positions of the top of the headrest pad are indicated with horizontal lines, with model baseline (Nij = 0.5) indicated in yellow font. Headrest height was varied in 2.5 cm increments. Results indicate that for all headrest positions where the top of the headrest pad was aligned at least 5 cm above the center of gravity of the head, the Nij response did not exceed the baseline value (Nij=0.5). The center of gravity of the head aligns with the tragion notch of the pinna (external ear) [13]. The superior aspect of pinna is approximately 3 cm above the tragion in adult males [14]. Thus, this minimum headrest height corresponds approximately to a headrest position where the top of the headrest pad is 2.5 cm (1”) above the top of the ears.
DISCUSSION
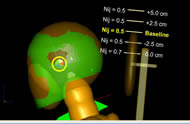
Figure 3: Nij response is displayed for five headrest heights. The baseline headrest height was determined such that the center of the headrest pad was in vertical alignment with the head center of gravity. The top surface of the headrest pad is indicated with horizontal lines. Baseline Nij value (0.5) is shown in yellow. Head center of gravity is highlighted with a yellow circle. (Click for larger view)
Current clinical practice to establish best headrest position is primarily determined on a case-by-case basis for those who need head support to improve function, positioning and comfort. The potentially protective effect of wheelchair-mounted headrest use in a motor vehicle impact has been previously reported [8]. Results from this computer simulation study indicate that wheelchair headrest position has a relationship to its ability to afford neck injury protection in a rear impact. A minimum height with the top of the headrest pad placed 2.5 cm (1 inch) above the top of the ear appears to effectively limit neck extension, reducing the likelihood of neck injury. Likewise, closer headrest proximity in the fore-aft direction reduces neck injury criteria outcomes. These results mirror the automotive literature that indicates optimal headrest placement limits neck extension and neck injury [15, 16].
Results from this study concur with the current recommendation to place the wheelchair-mounted headrest in close proximity to the head during transportation in a motor vehicle [7]. These results expand upon the current recommendation to position the headrest such that the middle of the headrest pad aligns with the top of the ears [7] by providing a minimum height. When possible, a headrest should be adjusted to meet these recommendations for travel in a motor vehicle.
Issues associated with biofidelity of the ATD limit all studies that use human surrogates. The ATD seated-posture resulted in an unnatural forward positioning of the head. The level of validation by MADYMO of the Hybrid III six-year old ATD model also limits this study. Yet, these surrogates represent the current state of the science for examining human response in potentially injurious scenarios. Comparing Nij response across similar scenarios mitigates physical and model ATD limitations.
Our results are particularly encouraging, as the effect of wheelchair-mounted headrest position on neck injury protection has not been previously studied. Existing recommendations have been based on principles of occupant protection and knowledge about the biomechanics of injuries. This study allowed quantitative comparisons of neck injury criteria based on headrest position and the results support and enhance current headrest positioning recommendations.
REFERENCES
- Department of Transportation, Rear Impact Protection: Rulemaking Public Meeting. 2002, National Highway Traffic Safety Administration,: Detroit, Michigan.
- U.S. Food and Drug Administration, 21cfr890 - Physical Medicine Devices. 2007, U.S. Food and Drug Administration: Washington D.C.
- Department of Transportation (DOT), FMVSS 202: Head Restraints for Passenger Vehicles. 2000: Washington D.C.
- Welcher, J.B. and Szabo, T.J., Relationships between Seat Properties and Human Subject Kinematics in Rear Impact Tests. Accident Analysis and Prevention, 2001. 33(3): p. 289-304.
- National Highway Traffic Safety Administration, FMVSS 213: Child Restraint Systems, Child Restraint Anchorage Systems. Vol. 49 CFR 571 and 596 Docket No. 98-3390. 1999.
- Fuhrman, S.I., Buning, M.E., and Karg, P. Prescription Patterns of Secondary Postural Support Devices and Concerns Related to Their Use During Vehicle Transportation. in RESNA Annual Conference. 2005. Atlanta, Georgia: RESNA.
- RERC on Wheelchair Transportation Safety, Guidelines for Use of Secondary Postural Support Devices by Wheelchair Users During Travel in Motor Vehicles. 2007: Pittsburgh, PA.
- Fuhrman, S.I., Karg, P., and Bertocci, G., Effect of Wheelchair Headrest Use on Pediatric Head and Neck Injury Risk Outcomes During Rear Impact. Accident Analysis and Prevention, 2008. 40(4): p. 1595–1603.
- Pipkorn, B. and Eriksson, M., A Method to Evaluate the Validity of Mathematical Models, Autoliv Research, Editor. 2003, TNO Automotive: Stockholm.
- Fuhrman, S.I., The Effect of Pediatric Wheelchair and Headrest Parameters on Relative Injury Risk under Rear Impact Conditions and Resulting Design Guidelines for Rear Impact Protection, in Rehabilitation Science and Technology. 2008, University of Pittsburgh: Pittsburgh. p. 292.
- King, A.I., Fundamentals of Impact Biomechanics: Part I - Biomechanics of the Head, Neck and Thorax. Annual Review of Biomedical Engineering, 2000. 2(1): p. 55-81.
- Kleinberger, M., et al. Effects of Head Restraint Position on Neck Injury in Rear Impact. 1999.
- Spitzer, C.R., The Avionics Handbook. 2001: CRC Press.
- Harry G. Armstrong Aerospace Medical Research Lab Wright-Patterson Afb Oh, Anthropometry and Mass Distribution for Human Analogues. Volume 1. Military Male Aviators. 1988: Defense Technical Information Center.
- Viano, D.C. and Gargan, M.F., Headrest Position During Normal Driving: Implication to Neck Injury Risk in Rear Crashes. Accident Analysis & Prevention, 1996. 28(6): p. 665-674.
- Farmer, C.M., Wells, J.K., and Werner, J.V., Relationship of Head Restraint Positioning to Driver Neck Injury in Rear-End Crashes. Accident Analysis & Prevention, 1999. 31(6): p. 719-728.
ACKNOWLEDGEMENTS
This work was funded in part by the National Institute on Disability and Rehabilitation Research (NIDRR), Rehabilitation Engineering Research Center (RERC) on Wheelchair Transportation, Grant # H133E010302 and in part by the National Science Foundation (NSF) Interdisciplinary Research Training in Assistive Technology (IGERT), Grant # DGE 0333420. The opinions expressed herein are those of the authors and are not necessarily reflections of the NIDRR or NSF.
This publication was also made possible in part by Grant Number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
AUTHOR INFORMATION
Susan I. Fuhrman / University of Pittsburgh 2310 Jane Street / Pittsburgh, PA 15203 412-586-6905 / Fax: 412-586-6910